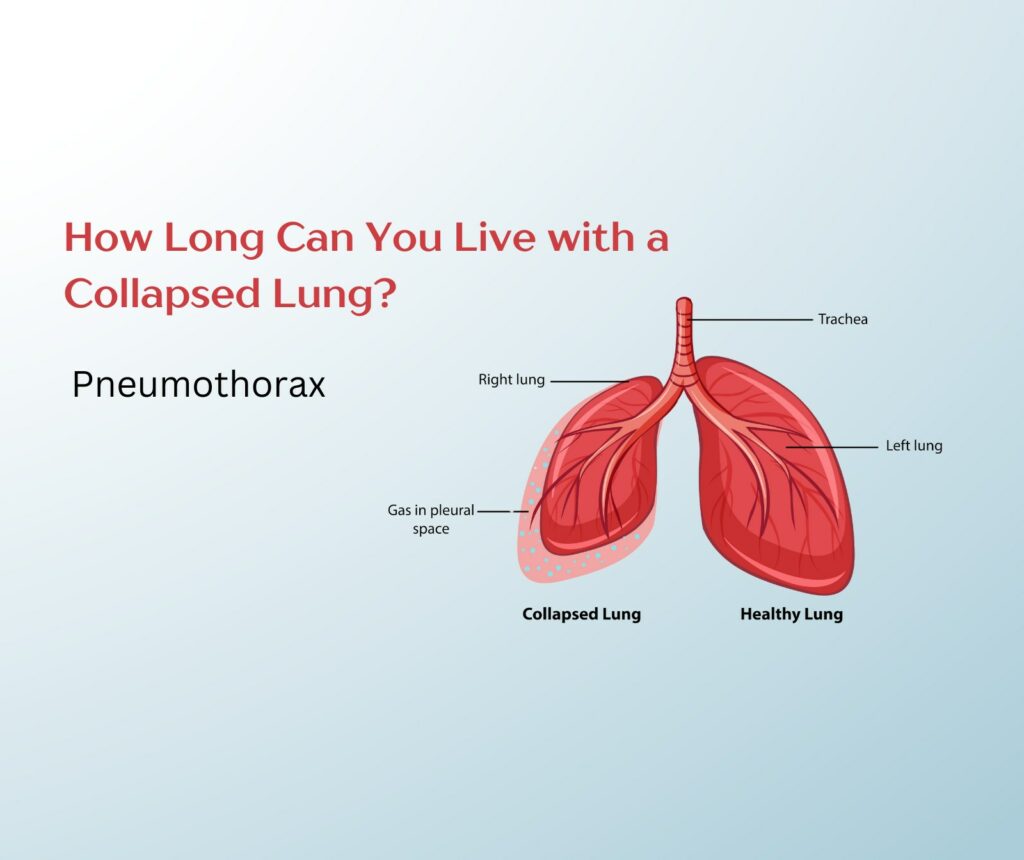
A collapsed lung can terrify patients and their families during a medical emergency. Being a Chest Surgeon many people ask me about their chances of survival and How Long Can You Live with a Collapsed Lung? The answer depends on several factors that affect each case differently.
Survival time with a collapsed lung (pneumothorax) depends on multiple elements. The severity of collapse plays a crucial role. The patient’s overall health condition matters too. Quick medical treatment makes the biggest difference in survival rates. A fully collapsed lung can threaten life within hours if left untreated.
Understanding Collapsed Lung Survival Timeframes
Collapsed lungs have different survival timeframes, and these windows are vital for patients and healthcare providers to understand. Let’s look at how long people can survive with different types of lung collapses.
Immediate survival window without treatment
Survival time without treatment changes based on how severe the collapse is. Here’s what we usually see:
- Minor partial collapse: People can survive for days to weeks with mild symptoms
- Complete collapse: The survival window shrinks to hours or days
- Tension pneumothorax: Requires immediate intervention, people only have minutes to hours to survive
Impact of different types of pneumothorax on survival
Death rates vary substantially between different types of pneumothorax. Patients between 15-40 years old have a low in-hospital death rate of 0.06-0.32%. The rate jumps to 8-18% in patients aged 70-95 years.
Critical factors affecting survival rates
These key factors determine survival outcomes:
- Speed of Medical Intervention: Quick care is vital, especially if you have tension pneumothorax
- Overall Health Status: Existing health conditions can affect your chances of survival
- Age and Physical Condition: Young and healthy people tend to recover better
- Extent of Collapse: Partial collapses give better survival rates than complete ones
Studies show that pneumonia with pneumothorax pushes the mortality rate up to 33%. People with underlying lung diseases face bigger risks. About 88.3% of cases happen to patients who already have pulmonary conditions.
Tension pneumothorax needs immediate medical help. This condition can lead to cardiovascular collapse and death faster without quick treatment. Most straightforward cases get better within 10 days with proper medical care.
Medical Intervention and Survival Rates
Our experience treating collapsed lungs shows that medical intervention timing is a vital factor in patient survival. The relationship between different treatments and survival rates demonstrates why timing matters so much.
Emergency treatment timeline
Patient survival depends on our immediate response to a collapsed lung case. Emergency needle decompression becomes necessary without delay for tension pneumothorax. Less severe cases give us several treatment options:
- Observation with oxygen therapy for small collapses
- Needle aspiration for moderate cases
- Chest tube insertion for severe cases
- Emergency surgery for complicated cases
Success rates of different interventions
Proper intervention leads to remarkable success rates. Needle aspiration achieves an 83% success rate, and the outpatient management approach lets 60% of patients go home within 4 hours. Chemical pleurodesis or surgery becomes our recommendation for persistent cases, which drops recurrence rates to less than 5%.
Impact of delayed treatment on survival
Timely treatment saves lives. Patient care delays lead to major complications. Research proves that surgery delayed beyond 38 days after diagnosis worsens survival outcomes. Tension pneumothorax cases can progress faster to cardiovascular collapse if left untreated.
Treatment timing and underlying conditions affect mortality rates by a lot. Secondary spontaneous pneumothorax has a 10% mortality rate, and tension pneumothorax shows higher death rates with delayed treatment. Most patients recover fully within 6 to 8 weeks with quick treatment.
Risk Factors Affecting Life Expectancy
Risk factors play a vital role in predicting survival outcomes for collapsed lung patients. Our extensive experience treating pneumothorax cases has helped us identify several factors that greatly affect life expectancy.
Pre-existing medical conditions
Our observations show that lung conditions have a dramatic effect on survival rates. Patients who have COPD make up about 70% of secondary pneumothorax cases. Research points to several conditions that increase vulnerability:
- Chronic respiratory diseases (COPD, cystic fibrosis)
- Infectious conditions (tuberculosis, pneumonia)
- Structural lung diseases (cancer, pulmonary fibrosis)
- Acute respiratory distress syndrome (ARDS)
Age and physical condition considerations
We’ve seen clear patterns in how age and physical characteristics shape survival outcomes. Young adults between 18-40 years show better recovery rates. A patient’s physical attributes matter too – tall, thin body types, especially in males, face higher risks.
Lifestyle factors impacting survival
Our data reveals several lifestyle factors that greatly affect survival rates. Smoking stands out as the biggest risk – heavy smokers have a 102 times higher risk of developing pneumothorax compared to non-smokers. We also keep track of other important factors:
- Drug use, particularly inhaled substances
- High-risk activities with pressure changes (flying, diving)
- Occupational exposures
The recurrence rates range from 20% to 60% within the first three years after the original episode. These numbers show why we strongly promote lifestyle changes and regular monitoring, especially when multiple risk factors exist.
Long-term Survival Prognosis
Our clinical data shows positive outcomes for most collapsed lung patients who receive proper care and monitoring. Let’s look at what patients can expect in their recovery.
Recovery timeline expectations
Most patients achieve full recovery within 6 to 8 weeks. The recovery experience typically follows these phases:
- First 48-72 hours: Lung re-expansion occurs
- First 2 weeks: Puncture site heals
- 6-8 weeks: Patient regains full functionality
Recurrence risks and survival implications
Our practice data reveals distinct recurrence patterns. The first year is vital with recurrence rates of 13% for males and 15% for females. The 5-year recurrence risk rises to 20% for males and 22% for females.
Surgical intervention substantially affects recurrence rates. Surgical pleurodesis prevents recurrence in more than 90% of cases. Young patients under 14 who undergo surgery face higher risks with recurrence rates up to 50%.
Long-term health monitoring requirements
Our team implements complete monitoring protocols for all collapsed lung patients. We focus on:
Regular checkups become vital since recurrence risks can last up to three years after the original episode. Patients who get prompt treatment rarely face long-term health complications. We recommend avoiding smoking and extreme pressure changes to reduce recurrence risks.
Conclusion
Patients with a collapsed lung need proper medical care and close monitoring. The recovery rates are impressive, and most people get back to their normal routines within 6-8 weeks after receiving quick treatment.
The numbers tell a positive story. Surgical procedures prevent the condition from coming back in more than 90% of cases. Standard treatments also work well if doctors start them early. A patient’s age, health conditions, and lifestyle choices can affect their recovery. Quick medical intervention significantly boosts their chances of getting better.
Doctors need to keep watching patients after they recover, especially in the first three years when the risk of relapse is highest. Our team’s experience shows that people who listen to their doctor’s advice and skip risky behaviors like smoking have the best chance of staying healthy. Regular checkups play a crucial role in long-term success.
FAQs
Q1. How long does it typically take to recover from a collapsed lung? Most patients can expect a full recovery within 6 to 8 weeks. The initial healing phase takes about 48-72 hours for lung re-expansion, followed by basic recovery in about 2 weeks, and complete recovery in 6-8 weeks for full functionality.
Q2. What are the common symptoms of a collapsed lung? Common symptoms include sharp chest or shoulder pain that worsens with deep breathing or coughing, shortness of breath, and in some cases, nasal flaring due to breathing difficulties.
Q3. Can a collapsed lung recur, and what are the risks? Yes, a collapsed lung can recur. The recurrence risk is about 13-15% within the first year and increases to 20-22% over five years. However, surgical interventions like pleurodesis can reduce recurrence rates to less than 10%.
Q4. Is it possible to have a collapsed lung without knowing it? In some cases, especially if the collapse happens slowly, there may be few or no noticeable symptoms. Mild symptoms might include shortness of breath, an increased heart rate, or a persistent cough that doesn’t seem to improve.
Q5. What factors affect survival rates for a collapsed lung? Survival rates are influenced by several factors, including the speed of medical intervention, overall health status, age, physical condition, and the extent of the lung collapse. Pre-existing lung conditions, smoking, and certain lifestyle factors can also significantly impact outcomes.
Pneumothorax Surgeon in Delhi – Dr. Pallavi Purwar
If you are struggling to find out How Long Can You Live with a Collapsed Lung? Dr. Pallavi Purwar can answer all your queries regarding your Lung Health. Dr Pallavi is a leading thoracic surgeon in Delhi, specialising in the treatment of pneumothorax (collapsed lung). With extensive experience and expertise, she provides advanced surgical solutions to manage this condition effectively, ensuring faster recovery and improved lung health. For expert care and personalized treatment, consult Dr. Pallavi Purwar today.