National Heart Institute, Holy Family Instititue
Sir Ganga Ram Hospital – Mon, Wed, Fri (8 AM – 10 AM) – F87 OPD Building (12 to 3 PM) at Room 2328
Thoracic Surgeon – New Delhi
MBBS, MS, Doctorate Thoracic Surgery
MBBS, MS, Doctorate Thoracic Surgery
Holy Family Hospital, National Heart Institute, Delhi Heart & Lung Institute, Kailash Hospital Noida, Apollo Spectra Kanpur, Delhi Chest Surgery
Thoracic Surgeon – New Delhi
MBBS, MS, Doctorate Thoracic Surgery
Understanding the Role of Pleural Effusion in Respiratory Diseases
Introduction
Pleural effusion is a common complication in various respiratory diseases, significantly impacting patient outcomes and quality of life. This article aims to provide a comprehensive understanding of pleural effusion’s role in respiratory diseases, its diagnosis, treatment, and recent advancements in management.What is Pleural Effusion?
Pleural effusion refers to the abnormal accumulation of fluid in the pleural space, the area between the lungs and the chest wall. This space normally contains a small amount of fluid for lubrication, but when excess fluid accumulates, it can impair lung function and cause respiratory distress [1].Pleural Effusion in Various Respiratory Diseases
Pneumonia
Pneumonia is one of the most common causes of pleural effusion. Approximately 40% of patients hospitalized with pneumonia develop a parapneumonic effusion [2]. These effusions can be categorized into three stages:- Exudative stage
- Fibrinopurulent stage
- Organizing stage
Lung Cancer
Malignant pleural effusion (MPE) is a common complication in lung cancer, occurring in approximately 15% of patients at the time of diagnosis and in up to 50% during the course of the disease [3]. MPE significantly impacts prognosis and quality of life. Recent studies have shown that the presence of MPE in non-small cell lung cancer (NSCLC) is associated with a median survival of 5.5 months [4].Congestive Heart Failure
Congestive heart failure (CHF) is a leading cause of transudative pleural effusions. In a study of 3,245 patients with CHF, 28% were found to have pleural effusions [5]. The mechanism involves increased hydrostatic pressure in the pulmonary circulation, leading to fluid accumulation in the pleural space.Other Respiratory Conditions
Pleural effusion can also occur in other respiratory conditions, including:- Tuberculosis
- Pulmonary embolism
- Mesothelioma
- Systemic lupus erythematosus
- Rheumatoid arthritis
Diagnosis and Treatment
Diagnosis of pleural effusion typically involves:- Physical examination
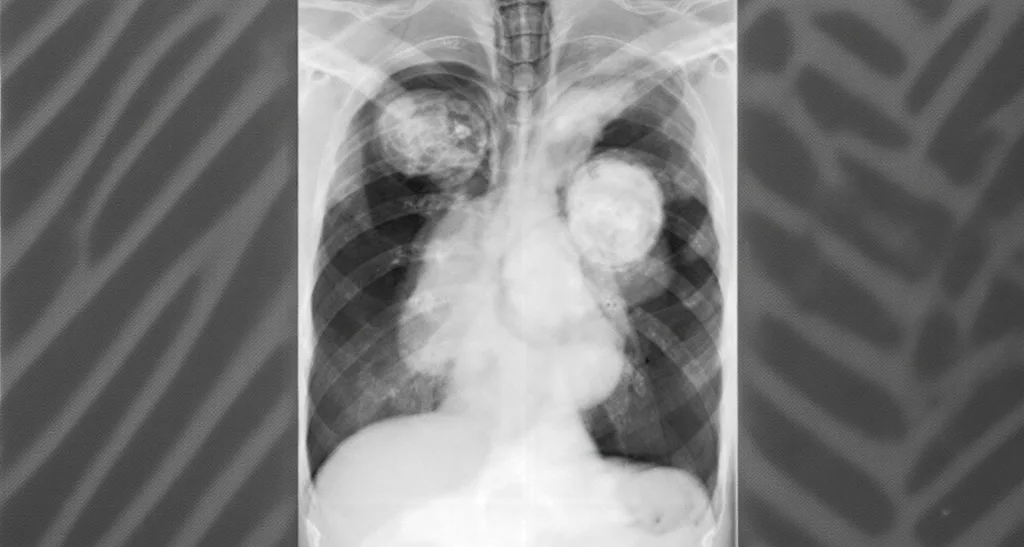
- Chest X-ray
- Ultrasound
- CT scan
- Thoracentesis for fluid analysis
- Antibiotics for infectious causes
- Diuretics for CHF-related effusions
- Thoracentesis for symptomatic relief
- Pleurodesis for recurrent malignant effusions
- Indwelling pleural catheters for long-term management
Recent Advancements
Recent advancements in the management of pleural effusions include:- Use of ultrasound-guided procedures for improved accuracy and safety [6]
- Development of novel biomarkers for differentiating between malignant and benign effusions [7]
- Implementation of rapid pleurodesis protocols for shorter hospital stays [8]
- Exploration of intrapleural fibrinolytic therapy for complicated parapneumonic effusions [9]
Case Studies
[Include 2-3 relevant case studies here]Frequently Asked Questions
- Q: What are the most common symptoms of pleural effusion? A: Common symptoms include shortness of breath, chest pain (especially when breathing deeply), dry cough, and fever. However, small effusions may be asymptomatic.
- Q: How is pleural effusion diagnosed? A: Diagnosis typically involves a combination of physical examination, chest X-ray, ultrasound, and CT scan. Thoracentesis may be performed to analyze the fluid.
- Q: Can pleural effusion be life-threatening? A: While not always life-threatening, large effusions can cause respiratory distress. Infected effusions (empyema) can be serious if left untreated.
- Q: How is pleural effusion treated? A: Treatment depends on the underlying cause. It may include addressing the primary condition, draining the fluid (thoracentesis), or in some cases, surgery.
- Q: Can pleural effusion recur after treatment? A: Yes, especially in cases of malignancy or chronic conditions. Recurrent effusions may require long-term management strategies like indwelling pleural catheters or pleurodesis.